Navigating the world of network providers and out-of-network costs can feel like decoding a secret language. Whether you’re trying to find the right doctor, schedule a specialist visit, or simply understand your medical bills, the maze of insurance jargon and surprise charges can quickly become overwhelming. But don’t worry — we’re here to make it easy! In this article, we’ll break down everything you need to know about network providers, what out-of-network really means, and how to avoid unexpected expenses. By the end, you’ll feel confident tackling your healthcare choices and keeping more money in your pocket. Let’s get started!
Table of Contents
- Understanding the Difference Between In-Network and Out-of-Network Providers
- How Out-of-Network Costs Can Impact Your Healthcare Budget
- Tips for Finding the Right Network Provider for Your Needs
- Smart Strategies to Minimize Unexpected Medical Bills
- To Wrap It Up
Understanding the Difference Between In-Network and Out-of-Network Providers
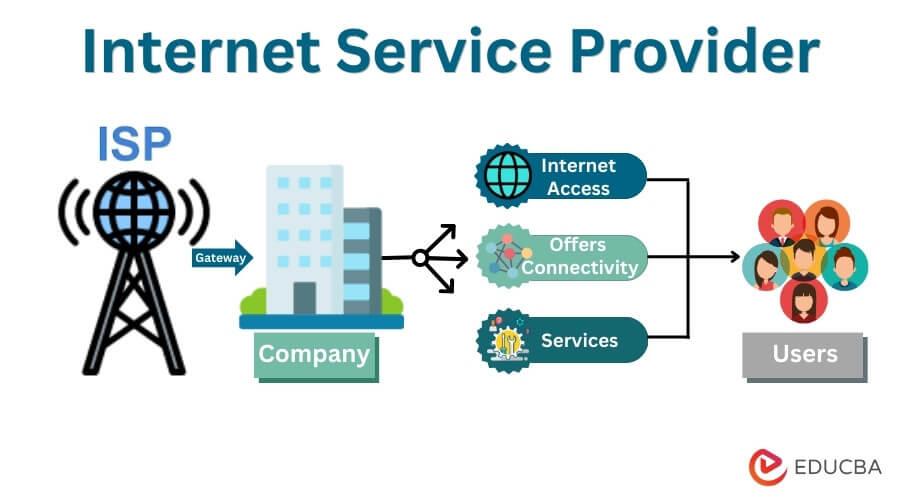
When it comes to choosing healthcare providers, understanding the distinction between in-network and out-of-network options can significantly impact your wallet. In-network providers have a contract with your insurance company, agreeing to accept negotiated rates for services. This means you’ll typically pay lower copayments, deductibles, and coinsurance fees. Using these providers ensures smoother claims processing and fewer unexpected bills, making your healthcare experience less stressful and more predictable.
On the flip side, out-of-network providers haven’t established a contract with your insurance company, which often results in higher costs. Insurance may cover only a portion of the expenses, leaving you to pay the rest, sometimes referred to as balance billing. Here’s what to keep in mind when considering out-of-network care:
- Higher out-of-pocket expenses
- Potential need for pre-authorization or referrals
- Greater risk of surprise medical bills
- A chance to access specialists not available in-network
Weighing these factors allows you to make informed choices, balancing care quality and cost-effectiveness while navigating your insurance benefits with confidence.
How Out-of-Network Costs Can Impact Your Healthcare Budget
When you seek care outside your insurance plan’s network, the financial impact can be surprisingly steep. Unlike in-network services, which usually have negotiated rates with your insurer, out-of-network care often means you’re billed at a higher, undiscounted rate. This leads to unexpected bills that can quickly blow up your healthcare budget. Unexpected out-of-pocket expenses like balance billing—where the provider charges you the difference between their fee and what your insurer pays—can catch many off guard. Understanding the cost difference beforehand can help you avoid these costly surprises.
Managing these expenses effectively means being proactive. Here are some tips to help you stay on track:
- Always verify network status of your healthcare providers before appointments.
- Request cost estimates if you anticipate needing out-of-network care.
- Explore options for partial reimbursements or appeals with your insurer.
- Consider supplemental insurance plans that cover some out-of-network costs.
Keeping these points in mind can make a huge difference in protecting your wallet while still getting the care you need.
Tips for Finding the Right Network Provider for Your Needs
Choosing a network provider is more than just picking the one with the lowest monthly premium. It’s essential to dive deep into the coverage details, including which hospitals and specialists are considered in-network. This can save you from unexpected medical bills that come with out-of-network services. Don’t forget to explore customer reviews and provider reputations – sometimes the best provider isn’t the cheapest but offers smoother claims processes and better customer service. Another tip is to verify if your preferred doctors or clinics accept the network plan you’re considering, ensuring continuity and comfort in your healthcare experience.
When evaluating options, keep an eye on the fine print about out-of-network costs. These expenses can quickly add up and derail your budget if you’re not prepared. Take advantage of online tools many providers offer to estimate out-of-pocket costs based on your specific health needs. Additionally, ask about any referral requirements or pre-authorization processes, which can affect both your expenses and access to care. By organizing your healthcare needs and comparing providers based on more than just price, you’ll confidently select a plan tailored to your lifestyle and peace of mind.
- Verify in-network doctors and hospitals you currently use or prefer
- Check customer satisfaction ratings and complaint records
- Understand out-of-network coverage caps and co-pays
- Utilize online cost calculators to anticipate expenses
- Ask about referrals and pre-authorization to avoid surprise bills
Smart Strategies to Minimize Unexpected Medical Bills
Understanding your health insurance network is the first line of defense against surprise medical expenses. Always confirm whether your healthcare provider is in-network before scheduling appointments or procedures. In-network providers have negotiated rates with your insurer, which often means substantially lower out-of-pocket costs for you. When you need urgent care or specialist services, checking network status ahead of time can save you from unexpected bills that come from out-of-network charges. Use your insurance company’s online directory or call customer service for quick verification.
Even with careful planning, out-of-network expenses can sometimes sneak up on you. To cushion the impact, consider these smart strategies:
- Request an Estimate: Before any procedure, ask your provider for a detailed estimate to avoid surprises.
- Negotiate Bills: If you receive a hefty out-of-network bill, don’t hesitate to negotiate or request a payment plan.
- Use an Advocate: Some insurers offer patient advocates who help manage billing concerns and disputes with providers.
- Opt for in-Network Tests: Whenever possible, ensure lab work and imaging services are performed within your network.
- Maintain Clear Records: Keep all bills and communications organized to spot errors or overcharges more easily.
To Wrap It Up
And there you have it—a straightforward guide to make sense of network providers and those pesky out-of-network costs. While it might seem daunting at first, understanding the basics can save you time, money, and stress down the road. Remember, a little research and asking the right questions go a long way in navigating your healthcare options with confidence. Here’s to making smarter choices and keeping your wallet—and your health—in good shape! Feel free to share your own tips or questions in the comments below; we’re all in this together. Happy navigating!